Why Does Anal Fistula Occur?
An anal fistula is characterized by tunnel-like structures around the anus filled with pus. This condition usually develops due to blockages and pus accumulation in the anal area, leading to abscess formation. Anal fistula is a chronic health issue that reduces the patient’s quality of life with symptoms such as pain during defecation, persistent discharge, and discomfort. If left untreated, the fistula deepens, the infection spreads, and treatment becomes more complex. Anal fistula has a high recurrence risk, especially in patients whose treatment is incomplete, making early diagnosis and intervention crucial to prevent progression.
Causes of Anal Fistula
While anal fistulas occur equally in both men and women, they can be more frequent with certain risk factors. Anal trauma, bowel diseases, straining during childbirth, and digestive disorders like Crohn’s disease are among the main causes. Diseases causing bowel inflammation or requiring surgery also increase fistula risk. A weakened immune system and the sensitivity of local tissues play a significant role, making it critical to understand potential triggers and seek early treatment.
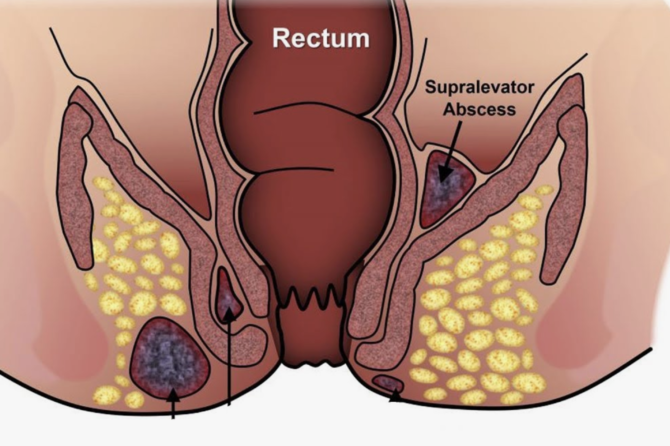
Reasons for Anal Fistula Formation
Anal fistulas develop from various factors, with blockages and infections as primary causes. Abscesses in the anal area lead to obstructions, which trigger fistula formation. If untreated, these abscesses form tunnel-like structures that continually discharge pus, causing symptoms like pain, swelling, and tenderness around the anus.
Crohn’s disease also contributes to anal fistula formation. This condition, which causes inflammation and thickening of the bowel walls, damages the digestive tract, creating a conducive environment for fistula formation. Additionally, people with weakened immune systems face increased infection risks, leading to higher incidences of anal fistulas.
Anal Fistula in Women
One of the causes of anal fistula in women is straining during childbirth. Long or strenuous deliveries can strain the muscles and tissues around the anus, increasing post-birth anal fistula risk. Additionally, some gynecological surgeries and vaginal procedures can lead to fistula development. Operations on the vaginal posterior wall may affect anal tissues, paving the way for fistula formation.
Other Causes
Sexually transmitted infections also contribute to anal fistula development. Diseases like HIV that weaken the immune system increase the risk. Additionally, treatments like radiation and chemotherapy in cancer patients may damage digestive tissues, aiding fistula formation. Medical interventions in the anal area, such as catheter use, may also lead to such conditions, as can minor traumas from surgeries around the anus.
What Helps Anal Fistula?
Antibiotics play a significant role in preventing infection spread and accelerating recovery. Physician-recommended antibiotics reduce inflammation and support healing. Anti-inflammatory and pain-relieving creams also help alleviate pain and discomfort but only provide temporary relief. Surgical intervention is necessary for a permanent solution.
Does Anal Fistula Heal on Its Own?
Anal fistulas do not heal spontaneously and become more complex over time. Thus, medical consultation is essential as soon as a fistula forms. Without treatment, the fistula deepens, creating additional tunnels and posing serious infection risks. Depending on its progression, medication or surgery may be recommended.
Can Anal Fistula Be Treated Non-Surgically?
With advances in medical technology, non-surgical methods like laser treatment are available for anal fistulas. Laser therapy involves burning and cleansing the infected tunnel, providing quick results with a fast recovery time and minimal risk of incontinence. Laser treatment stands out as an effective, alternative option for anal fistula treatment.
Anal fistula is a condition not to be overlooked; with early diagnosis and treatment, future health complications can be prevented.
Leave a reply

Leave a reply